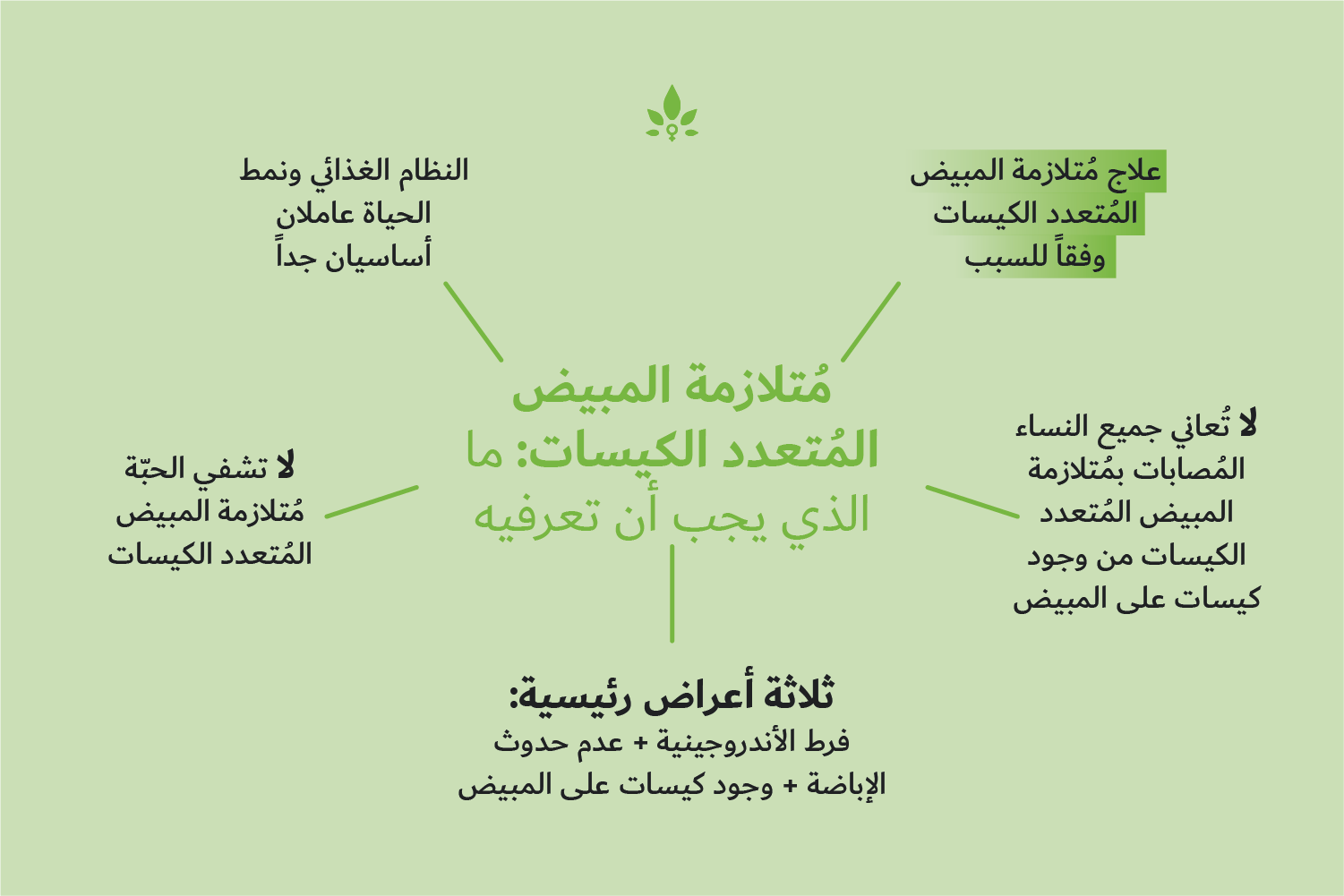
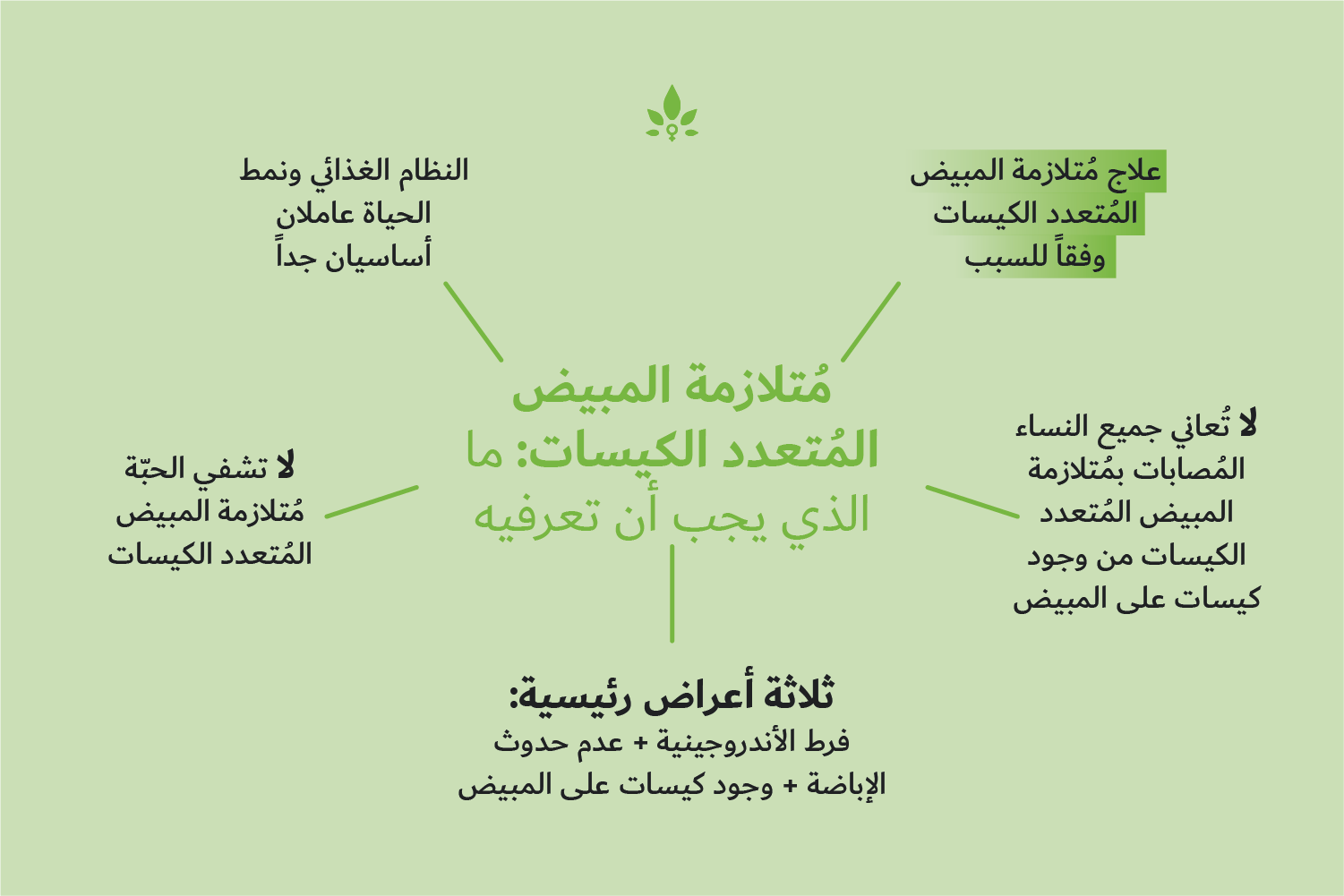
لماذا ينبغي علاج مُتلازمة المبيض المُتعدد الكيسات وفقاً للسبب؟
Polycystic Ovary Syndrome (PCOS) is the most common endocrine disorder affecting females of reproductive age. There is an urgent need for a better understanding of the condition because, if not managed successfully, the full impact of the associated symptoms of PCOS can be felt well beyond the menopause. Despite this, PCOS remains not particularly well understood and, in many cases, not particularly well managed clinically.
A multi-faceted condition
One major problem clinicians have is that there is no single causative factor that leads to the development of PCOS. Rather, it is likely to occur due to a complex interplay between various factors, including, but not limited to, genetic susceptibility, environmental factors, dysregulated hormone levels and metabolic status.
If we take a step back from diagnosing PCOS as a standalone condition and instead characterise it according to its predominant symptom or likely cause, we will be in a far better position to successfully manage the negative effects.
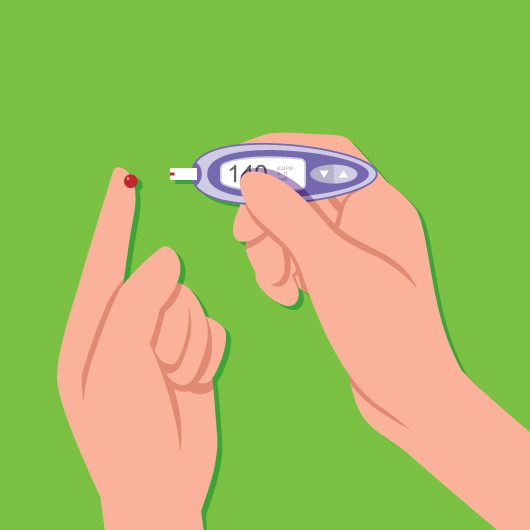
Insulin resistance
Whilst insulin resistance is not one of the main diagnostic criteria in PCOS, it is very common in females with the condition. In fact, insulin resistance affects up to 70% of women with PCOS and an increase in circulating insulin levels probably contributes to at least two of the three major clinical symptoms of the condition: hyperandrogenism and menstrual irregularities.
As insulin resistance becomes increasingly common globally, the incidence of PCOS is expected to increase. However, by making lifestyle changes, such as losing weight and eating a balanced diet, your risk of becoming insulin resistant is reduced and any associated PCOS symptoms should also be alleviated.
Other medical situations that can result in PCOS-like symptoms
Insulin resistance is not the only cause of PCOS-like symptoms. Thyroid disease, zinc deficiency and coming off the oral contraceptive pill can all contribute to symptoms that resemble those of PCOS. For a detailed review on all of these, click here.
It is important that your doctor rules out any of these conditions before committing to a diagnosis of PCOS, because treatment strategies will differ depending on the underlying cause. For example, women who have an underactive thyroid gland will usually find that thyroid medication manages their hypothyroidism and relieves their symptoms.
Women who have an excess of male hormones might find that their resulting hyperandrogenism is due to an adrenal disorder such as micronodular adrenocortical hyperplasia. This happens when the excess androgens are secreted by the adrenal gland, rather than the ovaries and will require different management to the ovarian androgen excess seen with traditional PCOS.
Why should treatment vary, dependent on cause?
Not every treatment option will be suitable for every woman with PCOS. The combined oral contraceptive pill is frequently prescribed to help with irregular menstrual cycles. However, as some oral contraceptives can actually increase insulin resistance, using the pill could easily exacerbate symptoms in a large subset of women with PCOS.
No single cause, means no single treatment and a personalised, multidisciplinary approach is the optimal method of managing any PCOS or PCOS-like symptoms.
To learn more about PCOS click here and try the PCOS Test to get more information.
Nabta is reshaping women’s healthcare. We support women with their personal health journeys, from everyday wellbeing to the uniquely female experiences of fertility, pregnancy, and menopause.
Get in touch if you have any questions about this article or any aspect of women’s health. We’re here for you.
Sources:
- Azziz, R, et al. “Positions Statement: Criteria for Defining Polycystic Ovary Syndrome as a Predominantly Hyperandrogenic Syndrome: an Androgen Excess Society Guideline.” The Journal of Clinical Endocrinology and Metabolism, vol. 91, no. 11, Nov. 2006, pp. 4237–4245., doi:10.1210/jc.2006-0178.
- De Melo, A S, et al. “Hormonal Contraception in Women with Polycystic Ovary Syndrome: Choices, Challenges, and Noncontraceptive Benefits.” Open Access Journal of Contraception, vol. 8, 2 Feb. 2017, pp. 13–23., doi:10.2147/OAJC.S85543.
- El Hayak, S, et al. “Poly Cystic Ovarian Syndrome: An Updated Overview.” Frontiers in Physiology, vol. 7, 5 Apr. 2016, p. 124., doi:10.3389/fphys.2016.00124.
- Gourgari, E, et al. “Bilateral Adrenal Hyperplasia as a Possible Mechanism for Hyperandrogenism in Women With Polycystic Ovary Syndrome.” The Journal of Clinical Endocrinology and Metabolism, vol. 101, no. 9, Sept. 2016, pp. 3353–3360., doi:10.1210/jc.2015-4019.
- “How Do Health Care Providers Diagnose PCOS?” National Institute of Health, www.nichd.nih.gov/health/topics/pcos/conditioninfo/diagnose. Last Reviewed Date 31/1/2017.
- Marshall, J C, and A Dunaif. “Should All Women with PCOS Be Treated for Insulin Resistance?” Fertility and Sterility, vol. 97, no. 1, Jan. 2012, pp. 18–22., doi:10.1016/j.fertnstert.2011.11.036.
- Niafar, M, and N D Nader. “Adiponectin as Serum Biomarker of Insulin Resistance in Patients with Polycystic Ovarian Syndrome.” Gynecological Endocrinology, vol. 31, no. 6, June 2015, pp. 473–476., doi:10.3109/09513590.2015.1008445.
- Norman, R J, et al. “The Role of Lifestyle Modification in Polycystic Ovary Syndrome.” Trends in Endocrinology and Metabolism, vol. 13, no. 6, Aug. 2002, pp. 251–257.
- Patel, S. “Polycystic Ovary Syndrome (PCOS), an Inflammatory, Systemic, Lifestyle Endocrinopathy.” The Journal of Steroid Biochemistry and Molecular Biology, vol. 182, Sept. 2018, pp. 27–36., doi:10.1016/j.jsbmb.2018.04.008.
- Polak, K, et al. “New Markers of Insulin Resistance in Polycystic Ovary Syndrome.” Journal of Endocrinological Investigation, vol. 40, no. 1, Jan. 2017, pp. 1–8., doi:10.1007/s40618-016-0523-8.
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. “Revised 2003 Consensus on Diagnostic Criteria and Long-Term Health Risks Related to Polycystic Ovary Syndrome.” Fertility and Sterility, vol. 81, no. 1, Jan. 2004, pp. 19–25.