What is Cushing’s Syndrome?


Cushing’s syndrome is named after the neurosurgeon, Mr. Harvey Cushing, who first described it in 1912. Patients with Cushing’s syndrome have too much cortisol. Fortunately very rare, it is a challenging condition to diagnose, with symptoms varying significantly, both in type and severity, between patients.
Cortisol is known as the ‘stress hormone’. It is produced by the adrenal glands and helps the body respond to stress. It is also involved in the regulation of blood sugar levels and blood pressure as well as reducing inflammation and modulating the immune system.
What causes Cushing’s syndrome?
Cushing’s syndrome can be exogenous or endogenous. Accurate management of the condition depends on first identifying the underlying cause of the disorder.
Exogenous Cushing’s syndrome affects people who take glucocorticoids (steroids). Steroids are an artificial version of cortisol. Those at most risk are patients with chronic health conditions, requiring long-term treatment; for example, asthma, rheumatoid arthritis and lupus. Steroids can also be used to manage pain and to suppress the immune system after transplant to reduce the risk of rejection.
Endogenous Cushing’s syndrome is caused by the body producing too much cortisol. This is usually a consequence of a tumour affecting either the pituitary gland, or the adrenal gland.
Adrenocorticotropic hormone (ACTH)-dependent Cushing’s syndrome comprises 80-85% of endogenous cases, with the majority of these attributable to tumours of the pituitary gland. The pituitary gland is located at the base of the brain. It is a small-pea-sized structure, responsible for secreting ACTH. ACTH tells the adrenal glands, located next to the kidneys, to produce cortisol. Too much ACTH results in too much cortisol. This form of ACTH-dependent Cushing’s syndrome is more accurately known as Cushing’s disease.
There are cases of tumours outside of the pituitary gland producing excess ACTH; this causes ectopic ACTH syndrome and can arise with lung tumours, as well as tumours of the pancreas and thyroid gland. Pituitary gland tumours are usually benign, but those that arise elsewhere in the body might be cancerous.
Adrenal gland tumours are ACTH-independent. 15-20% of endogenous Cushing’s syndrome occurs as a result of excess cortisol production due to tumours of the adrenal glands.
Who is most at risk of developing Cushing’s syndrome?
Cushing’s syndrome is very rare. It is estimated that the endogenous form of the condition affects between 0.7 and 2.4 people per million per year. It seldom affects children and is approximately three times more prevalent in women than men. The majority of cases are sporadic, although a small number of pituitary tumours have a genetic basis.
What are the most common symptoms of Cushing’s syndrome?
One of the biggest challenges with diagnosing Cushing’s syndrome is that the symptoms are nonspecific and can differ significantly between patients. Some of the most common are listed below:
- Weight gain; generally limited to the chest and abdomen region. In fact, the arms and legs can appear abnormally thin in contrast.
- Red puffy, rounded face.
- ‘Buffalo hump’ – a build-up of fat around the back of the neck and shoulders.
- Stretch marks (> 1cm), particularly across the abdomen, the breasts and the hips.
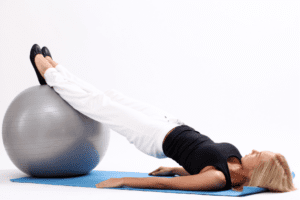
- Weakness in the arms and legs.
- Excessive hair growth.
- Bruising easily.
- Low libido and fertility problems. Women may experience irregular periods; men are become more susceptible to erectile dysfunction.
- Depression and mood swings.
- High blood pressure.
It also predisposes a person to other health issues, including:
- Heart attacks and strokes.
- Blood clots.
- Infections.
- Bone loss and fractures.
- Insulin resistance and type 2 diabetes.
- High cholesterol levels.
How is Cushing’s syndrome diagnosed?
In some cases it is necessary to rule out other medical conditions before committing to a diagnosis of Cushing’s syndrome. In women, it presents with many of the symptoms that are synonymous with Polycystic Ovary Syndrome (PCOS). Women with PCOS frequently experience irregular menstrual cycles as well as physical signs of hyperandrogenism, including hirsutism and acne. They are also susceptible to developing insulin resistance and becoming obese, both of which are risks for those with Cushing’s syndrome.
Another issue that can make diagnosing Cushing’s syndrome a challenge is in cases of ‘cyclical Cushing’s’, this is where the levels of cortisol vary, so a person does not always have higher than normal levels. They may, however, still exhibit some of the physical manifestations of the condition.
If your doctor suspects Cushing’s syndrome they will check your cortisol levels. Cortisol can be measured in the urine, blood and saliva. Often measurements will be taken over a 24 hour period because in healthy people cortisol levels drop in the evening. People with Cushing’s syndrome do not experience this decline in levels. Some people with suspected Cushing’s syndrome will be given a low dose of dexamethasone, which is a glucocorticoid. Doctors will then measure cortisol levels in the blood, with the expectation that low dose steroids should cause a lowering of endogenous cortisol levels. Levels remain high in patients with Cushing’s syndrome.
Once high cortisol levels are identified, in order to devise the most appropriate treatment plan, your doctor will need to determine what the cause of your Cushing’s syndrome is. This may be straightforward if you have been a long-term user of medicinal steroids, as your condition is likely to be directly related to this.
Endogenous Cushing’s syndrome can be more challenging to accurately diagnose. Blood tests will be utilised to identify whether your syndrome is ACTH-dependent or independent. If measured levels of ACTH are low, the most likely cause is an adrenal tumour (ACTH-independent); higher levels suggest a pituitary (or ACTH-secreting ectopic) tumour. The response to a shot of corticotropin-releasing hormone (CRH) can determine whether a tumour is pituitary or ectopic. CRH will increase the levels of ACTH and cortisol in those patients with a pituitary tumour, but not in those with an ectopic tumour.
Sometimes scans (MRI and/or CT) are performed in an attempt to visualise and localise any tumours. These have variable success rates depending on the size and location of the tumour. Pituitary tumours are usually very small and are easily missed by the most commonly used imaging techniques. An alternative approach is to take a sample of blood from the petrosal sinuses, which are the veins that are responsible for draining the pituitary gland. At the same time a blood sample will be taken from elsewhere in the body. If levels of ACTH are higher in the sample taken from the petrosal sinus than the other sample, a pituitary tumour is more likely; if levels are consistent across the two samples an ectopic tumour is the more likely cause.
What are the treatment options for Cushing’s syndrome?
As described above, diagnosing Cushing’s syndrome can be a convoluted process. Even once a positive diagnosis is reached, your doctor is likely to spend considerable time attempting to understand the specifics of your condition. This is all done to enable the most appropriate treatment strategy to be implemented. Cushing’s syndrome can be serious, and even fatal, if not treated. Thus, identifying the best management approach is essential.
If the syndrome is due to long-term use of steroids, your doctor will likely work with you to gradually reduce, or even stop altogether, your medication. It is imperative that you work with your doctor on this and do not attempt to self-wean off any medication.
If the underlying cause is because of a tumour, surgery and radiotherapy are the two main approaches. The treatment of pituitary tumours with surgery has a particularly high success rate, as high as 90% with an experienced surgeon. In some cases, the sudden drop in cortisol levels can cause an initial worsening of symptoms, as your body takes time to readjust. If the adrenal glands are removed, you will need to take medication for the rest of your life to replace the cortisol, and other hormones, that are no longer produced.
Pituitary and adrenal tumours are usually benign; but ectopic tumours can be cancerous and, if this is found to be the case, may require additional treatment, such as chemotherapy and more extensive surgical procedures.
Nabta is reshaping women’s healthcare. We support women with their personal health journeys, from everyday wellbeing to the uniquely female experiences of fertility, pregnancy, and menopause.
Get in touch if you have any questions about this article or any aspect of women’s health. We’re here for you.
Sources:
- Barnett, Richard. “Cushings Syndrome.” The Lancet, vol. 388, no. 10045, 13 Aug. 2016, p. 649., doi:10.1016/s0140-6736(16)31280-6.
- “Cushing’s Syndrome.” NHS Choices, NHS, www.nhs.uk/conditions/cushings-syndrome/.
- “Cushing’s Syndrome.” National Institute of Diabetes and Digestive and Kidney Diseases, U.S. Department of Health and Human Services, 1 May 2018, www.niddk.nih.gov/health-information/endocrine-diseases/cushings-syndrome.
- Sharma, Susmeeta, et al. “Cushing’s Syndrome: Epidemiology and Developments in Disease Management.” Clinical Epidemiology, vol. 7, 17 Apr. 2015, pp. 281–293., doi:10.2147/clep.s44336.