Getting Started with Nabta Health: Your 101 Guide to Fertility
Iman Saad • August 30, 2022 • 5 min read


Deciding you want to become pregnant and have a baby can be an incredibly exciting and overwhelming time. Fertility can be affected by many factors and there are ways to increase your chances of conceiving naturally. However, for some trying for a baby may not go as hoped or planned, and they might need further medical assistance to conceive.
Wherever you are on your fertility journey, Nabta Health will support you with resources, knowledge, and access to experts.
How can I increase my chances of getting pregnant naturally?
First things first. There are lifestyle steps you can take in the months before you start trying for a baby to prepare your body for conception.
- Take prenatal vitamins: To ensure your body is nutritionally strong, with all the minerals and vitamins you need for strong fetal development, start taking prenatal vitamins with folic acid at least three months before you try to conceive.
- Follow a balanced diet: Boost your health with a varied diet covering all food groups. Avoid refined sugars, saturated fats and too much salt.
- Maintain a healthy weight: Being underweight or overweight can impact fertility.
- Exercise regularly: Exercise that builds strength, endurance and muscle tone will help your body stay healthy and strong during pregnancy and labour.
- Get lots of rest and sleep: Sleep patterns can affect hormones. Stick to a regular 7-8 hours sleep routine as you prepare your body to conceive.
- Reduce stress: High stress levels are linked with difficulties getting pregnant. Give yourself a break when you can and take the pressure off. If you’re feeling frazzled, try taking up yoga and practice mindfulness.
- Stop smoking and quit drugs. Limit alcohol intake and cut back on caffeine.
- Come off contraception: If you’re on hormonal contraception (the pill, IUD, patch, ring implant) it can take some months for your body to readjust and your cycles to return to your personal ‘normal’. Of course, this doesn’t apply if you use condoms or a diaphragm for contraception as they simply act as a barrier to conceiving.
- Get a well-woman health check: Consider getting a full medical, including a check-up for any sexually transmitted infections (STIs). While this is by no means essential, your healthcare team will help you manage any potential red flags, family medical history or underlying health conditions that could af you getting pregnant naturally or having a healthy pregnancy.
How do women become pregnant?
The traditional way for heterosexual couples to get pregnant is through unprotected sexual intercourse.
Pregnancy is a question of timing (among other individual factors). Heterosexual couples who want to get pregnant will need to time sex with ovulation. The man’s sperm must meet and fertilise the egg at the right time. Knowing her fertile window and timing intercourse with ovulation is one of the most important factors in increasing a woman’s chances of conceiving.
What is ovulation?
The ovaries release the egg once every cycle, during ovulation. That egg travels down the fallopian tubes and waits to be fertilised by a sperm. The egg can wait for 12-24 hours for a sperm to successfully push through its outer surface. Sperm can live inside the female reproductive tract for 3-5 days waiting to fertilise an egg. All being good the fertilised egg makes its way to the uterus (womb) and implants in the uterine lining.
How do I know when I’m ovulating?
Women typically ovulate around 12 to 14 days before their next period. If you have regular periods (the average menstrual cycle is 28 days but it’s normal for women’s cycles to be anywhere from 21 to 40 days) you can count back from the first day of when you would expect your next period.
Fertility experts recommend having sex at least every other day in the lead-up to ovulation. Sperm can survive for several days in the female reproductive tract but once you’ve ovulated your egg has a 12-24 window for fertilisation so for the best chances of conception have enough sex in the time leading up to that brief window.
What is fertility awareness and natural family planning?
Fertility awareness methods (FAMs), also known as natural family planning, is used by women both as a method of contraception and to predict when they are most likely to conceive.
Women can monitor several physiological cues alongside tracking menstrual cycle length to determine when they are most fertile:
- Checking cervical mucous: Understanding how your cervical mucous changes during your cycle. As you near ovulation you’ll notice your discharge becomes clear, stretchy, and wet, with the consistency of raw egg whites. This is known as fertile quality mucous and you are now at your most fertile.
- Charting your basal body temperature (BBT): There is a small rise in body temperature after ovulation. Measuring your BBT can help you predict the exact point of ovulation. Women with regular periods can measure BBT for 3-4 cycles to gain a fairly accurate prediction of when they are most fertile
- Monitoring cervical mucous and BBT are non-invasive, easily accessible methods to track fertility. Using these two approaches together is known as the symptothermal method.
Other methods for tracking ovulation include:
- Calendar method: This works by recording menstrual cycles on a calendar for 6-12 months and calculating fertile periods. It is most effective as a fertility predictor when combined with cervical mucous and BBT methods.
- Ovulation predictor kits: Over the counter ovulation kits work in a similar way to at-home pregnancy tests. The woman pees on a stick measuring luteinizing hormone and a surge in this hormone indicates ovulation. However, it doesn’t prove an egg has been released and a woman can have the hormone surge but fail to ovulate.
- Period tracker apps: Smartphone ovulation tracker apps, like OvuSense, monitor menstrual cycles and predict fertility. If you do choose to use a smartphone tracker app, be sure to read the small print for data collection policies.
Fertility awareness, knowing and understanding your body and its menstrual cycles, helps lots of couples to conceive. However, getting pregnant isn’t always as simple as knowing your body and having lots of ‘baby making sex’. Some women want children but either cannot conceive naturally or keep miscarrying.
And obviously, there are different considerations for women who have irregular periods due to endometriosis or PCOS, those whose fertility is affected by illness or genetic history, and people who are single, transgender, or in same-sex relationships.
What affects female fertility?
Egg numbers and quality start to decline after 35, increasing the risk of age-related infertility. The risk of pregnancy-related complications also increases with age. Underlying health issues, endometriosis, uterine polyps or fibroids, polycystic ovarian syndrome (PCOS), problems with the fallopian tubes, and ovulatory problems can all affect fertility.
What affects male fertility?
Male fertility problems can be caused by low sperm count, poor quality sperm, or blockages preventing sperm moving through the reproductive tract. Sperm can be vulnerable to lifestyle and environmental factors including raised body temperature, weight gain, exposure to toxins, smoking, heavy alcohol intake and drug use.
What if I can’t get pregnant naturally?
Doctors define infertility as the inability to conceive after one year or longer of regular unprotected sex.
If you are a woman in a heterosexual relationship and struggling to conceive using fertility awareness and natural family planning methods, both you and your partner should seek a medical and physical evaluation.
In some situations, if a woman is 35 years or older, doctors may decide to investigate and treat infertility after 6 months of unprotected intercourse.
Fertility testing for women
Testing will depend on individual health and medical history, but typically initial testing will include routine blood work to check for:
-
Anti-Müllerian Hormone (AMH): Ovarian reserve test to estimate how many eggs a woman has.
-
Follicle-Stimulating Hormone (FSH): Hormone stimulates the follicle producing the eggs.
-
Luteinizing Hormone (LH): Responsible for follicle production and egg maturation.
-
Prolactin (PRL): Hormone released from anterior pituitary gland, raised during pregnancy in preparation for breastfeeding, and in women with infrequent periods.
-
Thyrotrophin (TSH): Can indicate an underactive thyroid, linked with irregular periods.
-
Estradiol: A form of estrogen, the test measures ovarian function and egg quality.
-
Androgen: High levels can prevent the ovaries from releasing an egg and may indicate polycystic ovarian syndrome (PCOS).
-
A Vaginal ultrasound will check:
- Reproductive organ health.
- Ovaries for cysts, fibroids, polyps, PCOS, endometriosis, or any abnormalities.
- Egg reserve.
Sometimes an X-ray is also carried out:
Hysterosalpingography (HSG): Examines inside of the uterus (womb) and fallopian tubes for blockages or anything that might be stopping the sperm from reaching the egg.
Fertility testing for men
Blood work for men will check hormone levels and scan for certain infections or a possible genetic cause for infertility. A doctor may request a sperm sample to assess sperm count, shape and movement, and a scrotal ultrasound to check if there are any problems or blockages in the testicles preventing sperm getting into a man’s ejaculate.
Fertility treatment options
Each person’s fertility scenario is unique, and any recommended infertility treatment will depend on an individual’s own health and medical history.
A woman with a blocked fallopian tube or a man who isn’t producing sperm will be offered procedures to remove the blockage, repair damage or retrieve sperm, before trying other fertility treatments.
If appropriate, fertility specialists will often recommend that women start with clomid, a prescribed oral medication for infertility. This is also the preferred approach for women with hormonal conditions such as polycystic ovarian syndrome (PCOS).
Clomid works by stimulating an increase in the levels of follicle-stimulating hormones, initiating ovulation and increasing the odds of pregnancy. For some women this approach is combined with intrauterine insemination (IUI), in which the male partner’s or donor’s sperm is inserted directly into the uterus to increase the probabilities of conception.
If that approach doesn’t work, or if it’s clear from a woman’s medical history it won’t work, the next step would be treatments such as in vitro fertilisation (IVF). IVF involves retrieving eggs from a woman’s body, fertilising the eggs in a laboratory, and transferring the resulting embryo back into her body. The process is lengthy, invasive, and expensive and can take an emotional toll. However, for many women who want children it is their only option.
Fertility treatments vary depending on a woman or couple’s situation. People who are single, in same-sex relationships or transgender will have their own fertility journeys and in these cases a woman’s age and fertility status still plays a role. Fertility experts will offer the necessary support and advice for each individual scenario.
Getting started on your fertility journey with Nabta Health
Whatever your personal situation, whether you’re thinking about starting a family, having another child, or you’ve been trying for years without success, Nabta Health will support you on your fertility journey.
From health and lifestyle tips for pre-conception and PCOS, to relationship coaching, pregnancy wellness products, and at-home vitamin, thyroid, and fertility testing, Nabta’s fertility marketplace and knowledge resources are designed to accompany you through each stage from pre-conception to birth.
Download the Nabta App
Related Articles

9 Natural Induction Methods Examined: What Does the Evidence Say?
Towards the end of [pregnancies](https://nabtahealth.com/article/ectopic-pregnancies-why-do-they-happen/), many women try methods of natural induction. The evidence supporting various traditional methods is variable, and benefits, side effects, and notable potential health risks are present. Understanding what science says can help individuals make informed choices in consultation with a provider. Induction of Natural Labour induction Myths, Realities and Precautions ---------------------------------------------------------------------- The following section will review nine standard natural induction methods, discussing the proposed mechanism, evidence, and safety considerations. Avoid potential hazards by avoiding risky labor triggers and get advice from your [obstetrician](https://nabtahealth.com/glossary/obstetrician/) before choosing any method mentioned below. Castor Oil ---------- Castor oil has been used throughout the centuries to induce labor, and studies suggest that it does so on some 58% of occasions. This oil stimulates prostaglandin release, which in turn may have the result of inducing cervical changes. Adverse effects, such as nausea and [diarrhea](https://www.mayoclinic.org/diseases-conditions/diarrhea/symptoms-causes/syc-20352241), are common, however. Castor oil should be used near the [due date](https://nabtahealth.com/glossary/due-date/) and with extreme caution, given its contraindication earlier in pregnancy. Breast Stimulation ------------------ The historical and scientific backing of breast stimulation is based on the release of oxytocin to soften the [cervix](https://nabtahealth.com/glossary/cervix/). A study has shown that, with this method, cervical ripening may be achieved in about 37% of cases. However, excessive stimulation may cause uterine hyperstimulation, and guidance from professionals may be essential. Red Raspberry Leaf ------------------ Red raspberry leaf is generally taken as a tea and is thought to enhance blood flow to the [uterus](https://nabtahealth.com/glossary/uterus/) and stimulate [contractions](https://nabtahealth.com/glossary/contraction/). Traditional use, however, is tempered by a relative lack of scientific research regarding its effectiveness. Animal studies have suggested possible adverse side effects, and no human data are available that supports a correlation with successful induction of labor. Sex --- Sex is most commonly advised as a natural induction method based on the principle that sex introduces [prostaglandins](https://nabtahealth.com/glossary/prostaglandins/) and oxytocin, and orgasm induces uterine [contractions](https://nabtahealth.com/glossary/contraction/). The few studies in the literature report no significant effect on labor timing. Generally safe for women when pregnancy is otherwise low-risk but may not speed labor. Acupuncture ----------- Acupuncture is a traditional Chinese practice that has been done to stimulate labor through the induction of hormonal responses. However, some studies show its effectiveness in improving cervical ripening but not necessarily inducing active labor. An experienced practitioner would appropriately consult its safe application during pregnancy. Blue and Black Cohosh --------------------- Native American groups traditionally utilize blue and black cohosh plants for gynecological use. These plants are highly discouraged nowadays from inducing labor because of the risk of toxicity they may bring. Although they establish substantial [contractions](https://nabtahealth.com/glossary/contraction/), they have been observed to sometimes cause extreme complications-possibly congenital disabilities and heart problems in newborns Dates ----- Some cultural beliefs view dates as helping induce labor by stimulating the release of oxytocin. They do not help stimulate uterine [contractions](https://nabtahealth.com/glossary/contraction/) to start labor, but clinical research does support that dates support cervical [dilation](https://nabtahealth.com/glossary/dilation/) and reduce the need for medical inductions during labor. They also support less hemorrhaging post-delivery when consumed later in pregnancy. Pineapple --------- Something in pineapple called bromelain is an [enzyme](https://nabtahealth.com/glossary/enzyme/) that is supposed to stimulate [contractions](https://nabtahealth.com/glossary/contraction/) of the [uterus](https://nabtahealth.com/glossary/uterus/). Animal tissue studies have determined it would only work if applied directly to the tissue, so it’s doubtful this is a natural method for inducing labor. Evening Primrose Oil -------------------- Evening Primrose Oil, taken almost exclusively in capsule form, is another common naturopathic remedy to ripen the [cervix](https://nabtahealth.com/glossary/cervix/). Still, studies are very few and indicate a greater risk of labor complications, such as intervention during delivery, and it is not recommended very often. Safety and Consultation ----------------------- Many of these methods are extremely popular; however, most are unsupported by scientific data. Any method should be discussed with a healthcare provider because all may be contraindicated depending on gestational age, maternal health, and pregnancy risk levels. Try going for a walk, have a warm bath and relax while you’re waiting for your baby. “Optimal fetal positioning,” can help baby to come into a better position to support labor. You can try sitting upright and leaning forward by sitting on a chair backward. Conclusion ---------- Natural methods of inducing labor vary widely in efficacy and safety. Practices like breast stimulation and dates confer some benefits, while others, such as those involving castor oil and blue cohosh, carry risks. Based on the available evidence, decisions about labor induction through healthcare providers are usually the safest. You can track your menstrual cycle and get [personalised support by using the Nabta app](https://nabtahealth.com/nabta-app/). Get in touch if you have any questions about this article or any aspect of women’s health. We’re here for you. Sources : 1.S. M. Okun, R. A. Lydon-Rochelle, and L. L. Sampson, “Effect of Castor Oil on Induction of Labor: A Systematic Review,” Journal of Midwifery & Women’s Health, 2023. 2.T. K. Ford, H. H. Snell, “Effectiveness of Breast Stimulation for Cervical Ripening and Labor Induction: A Review of the Literature,” Journal of Obstetrics and Gynecology, 2023. 3.R. E. Smith, D. M. Wilson, “Red Raspberry Leaf and Its Role in Pregnancy and Labor: A Critical Review,” Alternative Medicine Journal, 2024. 4.A. L. Jameson, “Sexual Activity and Its Effect on Labor Induction: A Review,” International Journal of Obstetrics, 2023. 5.B. C. Zhang, Z. W. Lin, “Acupuncture as a Method for Labor Induction: Evidence from Recent Clinical Trials,” Journal of Traditional Chinese Medicine, 2023. 6.D. K. Patel, J. M. Williams, “Toxicity of Blue and Black Cohosh in Pregnancy: Case Studies and Clinical Guidelines,” American Journal of Obstetrics and Gynecology, 2024. 7.M. J. Abdullah, F. E. Azzam, “The Role of Dates in Pregnancy: A Review of Effects on Labor and Birth Outcomes,” Nutrition in Pregnancy, 2024. 8.S. L. Chung, L. M. Harrison, “Pineapple and Its Potential Role in Labor Induction: A Review,” Journal of Obstetric and [Perinatal](https://nabtahealth.com/glossary/perinatal/) Research, 2023. 9.L. M. Weston, A. R. Franklin, “Evening Primrose Oil for Labor Induction: A Comprehensive Review,” Journal of Alternative Therapies in Pregnancy, 2024. Patient Information Induction of labour Women’s Services. (n.d.). Retrieved November 9, 2024, from https://www.enherts-tr.nhs.uk/wp-content/uploads/2019/10/Induction-of-Labour-v5-09.2020-web.pdf

Gynoid Fat (Hip Fat and Thigh Fat): Possible Role in Fertility
Gynoid fat accumulates around the hips and thighs, while android fat settles in the abdominal region. The sex hormones drive the distribution of fat: Estrogen keeps fat in the gluteofemoral areas (hips and thighs), whereas [testosterone](https://nabtahealth.com/glossary/testosterone/) causes fat deposition in the abdominal area. Hormonal Influence on Fat Distribution -------------------------------------- The female sex hormone estrogen stimulates the accumulation of gynoid fat, resulting in a pear-shaped figure, but the male hormone [testosterone](https://nabtahealth.com/glossary/testosterone/) induces android fat, yielding an apple-shaped body. Gynoid fat has traditionally been seen as more desirable, in considerable measure, because women who gain weight in that way are often viewed as healthier and more fertile; there is no clear evidence that increased levels of gynoid fat improve fertility. Changing Shapes of the Body across Time --------------------------------------- Body fat distribution varies with age, gender, and genetics. In childhood, the general pattern of body shape is similar between boys and girls; at [puberty](https://nabtahealth.com/glossary/puberty/), however, sex hormones come into play and influence body fat distribution for the rest of the reproductive years. Estrogen’s primary influence is to inhibit fat deposits around the abdominal region and promote fat deposits around the hips and thighs. On the other hand, [testosterone](https://nabtahealth.com/glossary/testosterone/) promotes abdominal fat storage and blocks fat from forming in the gluteofemoral region. In women, disorders like [PCOS](https://nabtahealth.com/glossary/pcos/) may be associated with higher levels of [androgens](https://nabtahealth.com/glossary/androgen/) including [testosterone](https://nabtahealth.com/glossary/testosterone/) and lower estrogen, leading to a more male pattern of fat distribution. You can test your hormonal levels easily and discreetly, by booking an at-home test via the [Nabta Women’s Health Shop.](https://shop.nabtahealth.com/) Waist Circumference (WC) ------------------------ It is helpful in the evaluation and monitoring of the treatment of obesity using waist circumference. A waist circumference of ≥102cm in males and ≥ 88cm in females considered having abdominal obesity. Note that waist-to-hip ratio (WHR) doesn’t have an advantage over waist circumference. After [menopause](https://nabtahealth.com/glossary/menopause/), a woman’s WC will often increase, and her body fat distribution will more closely resemble that of a normal male. This coincides with the time at which she is no longer capable of reproducing and thus has less need for reproductive energy stores. Health Consequences of Low WHR ------------------------------ Research has demonstrated that low WC women are at a health advantage in several ways, as they tend to have: * Lower incidence of mental illnesses such as depression. * Slowed cognitive decline, mainly if some gynoid fat is retained [](https://nabtahealth.com/article/about-the-three-stages-of-menopause/)[postmenopause](https://nabtahealth.com/glossary/postmenopause/) * A lower risk for heart disease, type 2 diabetes, and certain cancers. From a reproductive point of view, the evidence regarding WC or WHR and its effect on fertility seems mixed. Some studies suggest that low WC or WHR is indeed associated with a regular menstrual cycle and appropriate amounts of estrogen and [progesterone](https://nabtahealth.com/glossary/progesterone/) during [ovulation](https://nabtahealth.com/glossary/ovulation/), which may suggest better fecundity. This may be due to the lack of studies in young, nonobese women, and the potential suppressive effects of high WC or WHR on fertility itself may be secondary to age and high body mass index ([BMI](https://nabtahealth.com/glossary/bmi/)). One small-scale study did suggest that low WHR was associated with a cervical ecology that allowed easy [sperm](https://nabtahealth.com/glossary/sperm/) penetration, but that would be very hard to verify. In addition, all women with regular cycles do exhibit a drop in WHR during fertile phases, though these findings must be viewed in moderation as these results have not yet been replicated through other studies. Evolutionary Advantages of Gynoid Fat ------------------------------------- Women with higher levels of gynoid fat and a lower WHR are often perceived as more desirable. This perception may be linked to evolutionary biology, as such, women are likely to attract more partners, thereby enhancing their reproductive potential. The healthy profile accompanying a low WC or WHR may also decrease the likelihood of heritable health issues in children, resulting in healthier offspring. Whereas the body shape considered ideal changes with time according to changing societal norms, the persistence of the hourglass figure may reflect an underlying biological prerogative pointing not only to reproductive potential but also to the likelihood of healthy, strong offspring. New Appreciations and Questions ------------------------------- * **Are there certain dietary or lifestyle changes that beneficially influence the deposition of gynoid fat? ** Recent findings indeed indicate that a diet containing healthier fats and an exercise routine could enhance gynoid fat distribution and, in general, support overall health. * **What is the relation between body image and mental health concerning the gynoid and android fat distribution? ** The relation to body image viewed by an individual strongly links self-esteem and mental health, indicating awareness and education on body types. * **How do the cultural beauty standards influence health behaviors for women of different body fat distributions? ** Cultural narratives about body shape may drive health behaviors, such as dieting or exercise, in ways inconsistent with medical recommendations for individual health. **References** 1.Shin, H., & Park, J. (2024). Hormonal Influences on Body Fat Distribution: A Review. Endocrine Reviews, 45(2), 123-135. 2.Roberts, J. S., & Meade, C. (2023). The Effects of WHR on Health Outcomes in Women: A Systematic Review. Obesity Reviews, 24(4), e13456. 3.Chen, M. J., & Li, Y. (2023). Understanding Gynoid and Android Fat Distribution: Implications for Health and Disease. Journal of Women’s Health, 32(3), 456-467. 4.Hayashi, T., et al. (2023). Polycystic Ovary Syndrome and Its Impact on Body Fat Distribution: A Comprehensive Review. Frontiers in Endocrinology, 14, 234-241. 5.O’Connor, R., & Murphy, E. (2023). Sex Hormones and Fat Distribution in Women: An Updated Review. [Metabolism](https://nabtahealth.com/glossary/metabolism/) Clinical and Experimental, 143, 155-162. 6.Thomson, R., & Baker, M. (2024). Body Image, Self-Esteem, and Mental Health: The Role of Fat Distribution. Health Psychology Review, 18(1), 45-60. 7.Verma, P., & Gupta, A. (2023). Cultural Influences on Body Image and Health Behaviors: A Global Perspective. International Journal of Environmental Research and Public Health ([MDPI](https://www.mdpi.com/journal/ijerph)), 20(5), 3021.

Fact or Fiction: Garlic Oil Helps Cure Ear Infections 2024
Garlic oil helps cure ear infections, natural [treatments](https://nabtahealth.com/) such as garlic oil are highly recommended as possessing antibacterial and antiviral properties. But does garlic oil live up to its reputation? The Science Behind Garlic and Ear Infections -------------------------------------------- Garlic has been used as a natural remedy for several centuries to cure various infections, among other ailments. The active ingredient, allicin, has been shown to exhibit antibacterial and antiviral properties that can help with the symptoms of an ear infection. A few studies confirm that allicin decreases the presence of certain bacteria and viruses, thus assisting in resolving the ear infection sooner. Yet anatomically, the ear makes this problematic as the tympanic membrane, or eardrum, acts to prevent direct delivery of oil or drops to the area of the middle ear where infections occur. 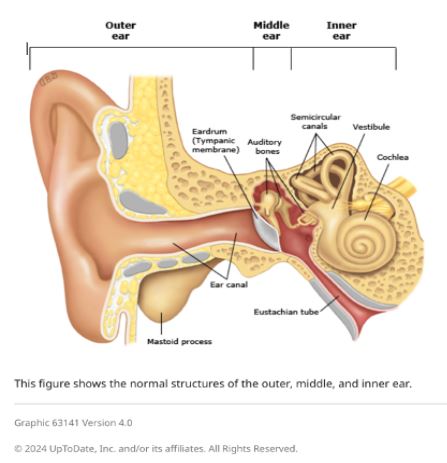 Evidence of Garlic Oil and Herbal Remedies ------------------------------------------ Studies on garlic oil, often combined with other herbs such as mullein, demonstrate it can decrease ear pain. A review published in 2023 reported that herbal ear drops, including those containing garlic, relieved pain in subjects with acute otitis media. However, researchers pointed out that while garlic oil may grant some advantages in the feeling of discomfort, its effect on the infection is limited by the eardrum barrier. Most infections will still self-resolve, but garlic oil can offer a natural alternative for pain management. Some studies in 2023 and 2024 also report that herbal extracts, including garlic, reduce dependence on heavy pain medications. Garlic is relatively cheaper and easier to access in herbal drops, particularly in many settings where prescription ear drops are not available. Safety and Proper Application of Garlic Oil ------------------------------------------- Being a potentially palliative resource, garlic needs to be used in the right manner. Experts advise against putting pure or undiluted garlic oil into the ear, as this can be too harsh and thus irritate or even injure sensitive ear tissue. Garlic extracts in commercially prepared herbal ear drops are recommended for use in the ear. In these products, garlic would have been diluted to safe levels while still being beneficial. Seeing a Health Professional ---------------------------- Consulting a health professional beforehand is very important when using garlic oil or any other herbal remedy against ear infections. Sometimes, ear infections result in complications, especially when not treated properly, and might cause recurrence. A healthcare provider will best help assess whether garlic oil or any other remedy may be indicated for each case and may recommend the safest treatment. Possible Benefits of Garlic Oil for Ear Health ---------------------------------------------- * Natural Pain Relief: Garlic oil’s antimicrobial and anti-inflammatory action soothes ear pain. * Cost-Effective: Garlic-based herbal remedies are generally cheaper than several prescription-based ear drops. * Readily Available Option: Garlic oil is readily available at health stores and can be ordered online. Current Research and Future Directions -------------------------------------- Herbal remedies, such as garlic oil, are still under research, especially for their role in pain relief and supporting natural recovery in light ear infections. Other studies investigate more advanced formulations that could let active compounds bypass the eardrum more effectively, thus giving a chance for enhanced effectiveness against middle-ear infections without the use of antibiotics. Key Takeaways ------------- * In effect, it has a minimal impact on the infection. It does not cure the disease but helps with earache because the membrane prevents the oil from reaching the middle ear. * Only use mild formulations. Commercially prepared herbal ear drops are very good compared to undiluted garlic oil. This is done to prevent irritation. * Consult a professional. Consult your health provider before this natural remedy, especially if you have recurring symptoms. References 1.Johnson, L., & Patel, R. (2023). [The Role of Herbal Remedies in Treating Ear Pain](https://pubmed.ncbi.nlm.nih.gov/): A Focus on Garlic Oil. Journal of Complementary Medicine, 61(2), 102-115. 2.Sharma, D., & Lee, H. (2024). Evaluating Garlic Extract for Natural Pain Relief in Ear Infections. Advances in Integrative Health, 42(1), 89-99. 3.Verhoeven, E., & Kim, S. (2023). Garlic and Herbal Extracts in Ear Infection Management. Health and Wellness Journal, 23(4), 167-178.

