What is Antiphospholipid Syndrome (APS)?

Antiphospholipid Syndrome is an autoimmune thrombophilia disorder seen more frequently in young women than in men. It leads to blood thickening and increased risk of blood clots developing in veins, arteries and the brain.
Linked with pregnancy complications and greater risk of miscarriage, conditions caused by APS include:
- Deep vein thrombosis (DVT) – a blood clot in the leg
- Arterial thrombosis – a clot in the artery which can cause stroke or heart attack
- Blood clots in the brain, leading to problems with mobility, memory, speech and vision.
APS is also known as Hughes or ‘sticky blood’ syndrome because those with APS are more prone to developing blood clots. The syndrome occurs in up to 1% of people and is four times more common in young women pre-menopause than in men.
What causes sticky blood syndrome?
Sticky blood syndrome happens when the immune system, which should be protecting and defending the body against bacteria, viruses and other pathogens, mistakenly attacks healthy tissues. ‘Abnormal’ blood proteins, antiphospholipid antibodies, attack the ‘normal’ antibody blood proteins produced by the immune system to fight infections. When the phospholipids are damaged inflammation and blood clots form in the veins and arteries.
It’s still not fully understood why autoimmune diseases occur or why more women are affected than men. It’s thought that genetics may play a role and a person’s (often unknown) underlying predisposition is activated by an infection or environmental trigger. APS comes under this umbrella and has been found to be present in people with systemic lupus erythematosus (lupus or SLE), another autoimmune disease. According to the National Heart, Lung and Blood Institute in the US, around 10% of people with lupus have APS, and about half of all people who have APS also have another autoimmune or rheumatic disorder.
What are the symptoms of APS and how is it diagnosed?
APS tends to be diagnosed when a person has recurrent early or late miscarriages, premature births, or blood clots that can’t be explained by anything else. The syndrome is also linked with stillbirth, pre-term birth, pre-eclampsia, fetal growth restriction (IUGR), and placental complications.
Your healthcare team will discuss your medical history and may suggest a blood test to detect whether the abnormal antiphospholipid antibodies that increase the risk of blood thickening are present in your body.
Warning signs you may have developed a blood clot include sudden pain and warmth in one leg or arm, chest pain, shortness of breath, blurred vision, weak or numb limbs, a blotchy rash or ulcers on the skin, and slurred speech. If you experience any of these symptoms you should contact your doctor immediately.
How does Antiphospholipid Syndrome affect pregnancy?
APS can cause serious pregnancy complications, the biggest concern being blood clots in the placenta. If blood clots develop in the placenta they may cut off blood supply to the baby, and with it oxygen, glucose and nutrients. Risks to the mother include thrombosis, pulmonary embolism, stroke and heart attack.
How is Antiphospholipid Syndrome managed during pregnancy?
While most women with clotting syndromes go on to have healthy pregnancies, if you are diagnosed as having APS before or during pregnancy you will be monitored as high-risk, with regular blood, urine, fetal heart rate and ultrasound tests and scans to check fetal and placental health.
Your medical team will recommend the safest delivery option for you and your baby and you may be prescribed daily blood-thinning medications such as aspirin or heparin during your pregnancy. Heparin is safe to continue taking post-birth if you choose to breastfeed your baby, or your doctor may prescribe warfarin which cannot be taken during pregnancy.
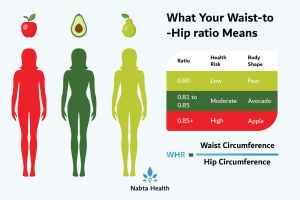
Your doctors will advise that certain lifestyle choices will also reduce your risk of developing blood clots, these include avoiding smoking, following a nutritionally-balanced diet and exercising regularly. You should also avoid long periods of sitting still and try to move around or stretch regularly on long trips.
___
Nabta is reshaping women’s healthcare. We support women with their personal health journeys, from everyday wellbeing to the uniquely female experiences of fertility, pregnancy, and menopause. You can track your menstrual cycle and get personalised support by using the Nabta app.
Get in touch if you have any questions about this article or any aspect of women’s health. We’re here for you.
Sources
John Hopkins Medicine “Autoimmune Disease: Why Is My Immune System Attacking Itself?” https://www.hopkinsmedicine.org/health/wellness-and-prevention/autoimmune-disease-why-is-my-immune-system-attacking-itself
National Heart, Lung and Bloog Institute “Antiphospholipid Antibody Syndrome” https://www.nhlbi.nih.gov/health-topics/antiphospholipid-antibody-syndrome
NHS, “Antiphospholipid Syndrome” https://www.nhs.uk/conditions/antiphospholipid-syndrome/
Tommy’s “Antiphospholipid syndrome (APS)” https://www.tommys.org/pregnancy-information/pregnancy-complications/antiphospholipid-syndrome-aps
Wittner, L et al “Antiphospholipid Syndrome (APS) in Pregnancy” East and North Hertfordshire, NHS Trust, April 2019 https://www.enherts-tr.nhs.uk/content/uploads/2019/10/Antiphospholipid-Syndrome-in-Pregnancy-Final-04.2019-web-1.pdf