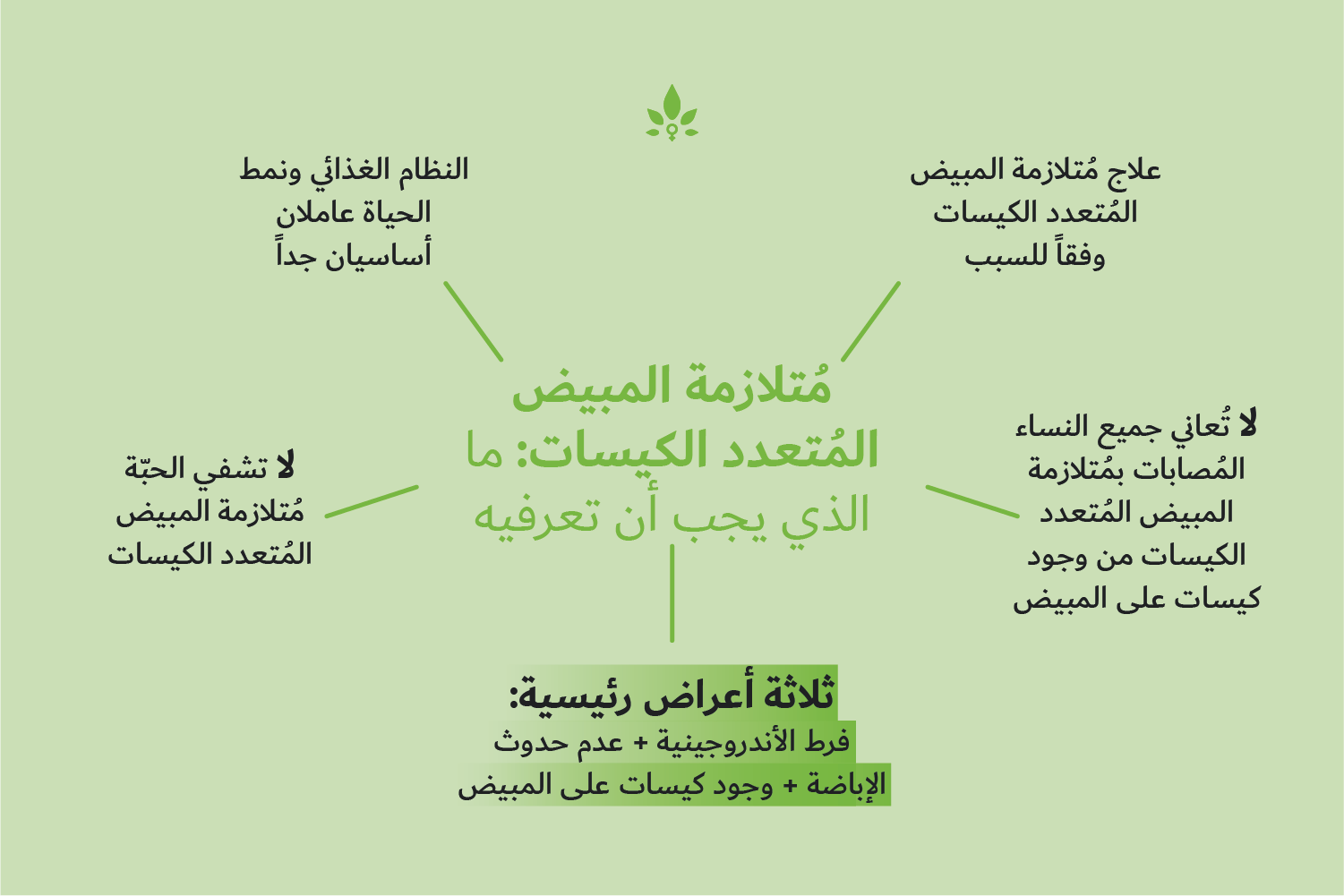
ما الذي يَربط بين فرط الأندروجينية، وعدم حدوث الإباضة، ووجود كيسات على المبيض؟
Many people have heard of Polycystic Ovary Syndrome (PCOS), but not everyone understands what the condition is and how it is diagnosed. The truth is, it can be very difficult, even for specialists in the field, to diagnose it and many women wait over two years to receive a positive diagnosis.
Guidelines for diagnosis
In 2003 the Rotterdam Consensus Workshop was established to redefine the optimum diagnostic criteria for PCOS, which had not been reviewed in detail since the National Institute of Health (NIH) established guidelines for diagnosis in 1990.
The outcome of the Rotterdam consensus was the identification of three clinical symptoms, experienced by many women with PCOS:
- Hyperandrogenism (an excess of male hormones)
- Menstrual cycle irregularity/anovulation
- Polycystic ovaries.
The consortium concluded that a patient should present with at least two of these symptoms before a positive PCOS diagnosis could be made. Since this consensus, both the NIH and the Androgen Excess Society have adopted very similar criteria, requiring two clinical signs for a PCOS diagnosis.
The review panels held subsequently have recognised a number of other common features of PCOS, including insulin resistance, obesity and elevated levels of luteinising hormone in the serum. Although their presence is often considered intrinsic to PCOS, none are yet recommended for use in its diagnosis.
Insulin resistance
Women with PCOS are considered to be at greater risk of developing insulin resistance. However, whether the insulin resistance results in, or is a consequence of, their PCOS remains unclear.
Insulin sensitivity does appear to contribute to many of the other symptoms of the condition; including hyperandrogenism, irregular menstruation, obesity and a predisposition to other metabolic conditions. Treating insulin resistance has also been shown to improve the symptoms of PCOS, providing further evidence that a deficiency in insulin signalling may be key to the pathogenesis of the condition in a large number of women.
To date though, the three defining features of PCOS remain those outlined by the Rotterdam consensus. Without two of these being present, a diagnosis of PCOS will not be made.
To learn more about PCOS click here.
Nabta is reshaping women’s healthcare. We support women with their personal health journeys, from everyday wellbeing to the uniquely female experiences of fertility, pregnancy, and menopause.
Get in touch if you have any questions about this article or any aspect of women’s health. We’re here for you.
Sources:
- Azziz, R, et al. “Positions Statement: Criteria for Defining Polycystic Ovary Syndrome as a Predominantly Hyperandrogenic Syndrome: an Androgen Excess Society Guideline.” The Journal of Clinical Endocrinology and Metabolism, vol. 91, no. 11, Nov. 2006, pp. 4237–4245., doi:10.1210/jc.2006-0178.
- El Hayak, S, et al. “Poly Cystic Ovarian Syndrome: An Updated Overview.” Frontiers in Physiology, vol. 7, 5 Apr. 2016, p. 124., doi:10.3389/fphys.2016.00124.
- “How Do Health Care Providers Diagnose PCOS?” National Institute of Health, www.nichd.nih.gov/health/topics/pcos/conditioninfo/diagnose. Last Reviewed Date 31/1/2017.
- Marshall, J C, and A Dunaif. “Should All Women with PCOS Be Treated for Insulin Resistance?” Fertility and Sterility, vol. 97, no. 1, Jan. 2012, pp. 18–22., doi:10.1016/j.fertnstert.2011.11.036.
- Polak, K, et al. “New Markers of Insulin Resistance in Polycystic Ovary Syndrome.” Journal of Endocrinological Investigation, vol. 40, no. 1, Jan. 2017, pp. 1–8., doi:10.1007/s40618-016-0523-8.
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. “Revised 2003 Consensus on Diagnostic Criteria and Long-Term Health Risks Related to Polycystic Ovary Syndrome.” Fertility and Sterility, vol. 81, no. 1, Jan. 2004, pp. 19–25.