هل يُمكن أن تُسبّب مُتلازمة المبيض المُتعدد الكيسات مشاكل بولية ومعوية؟
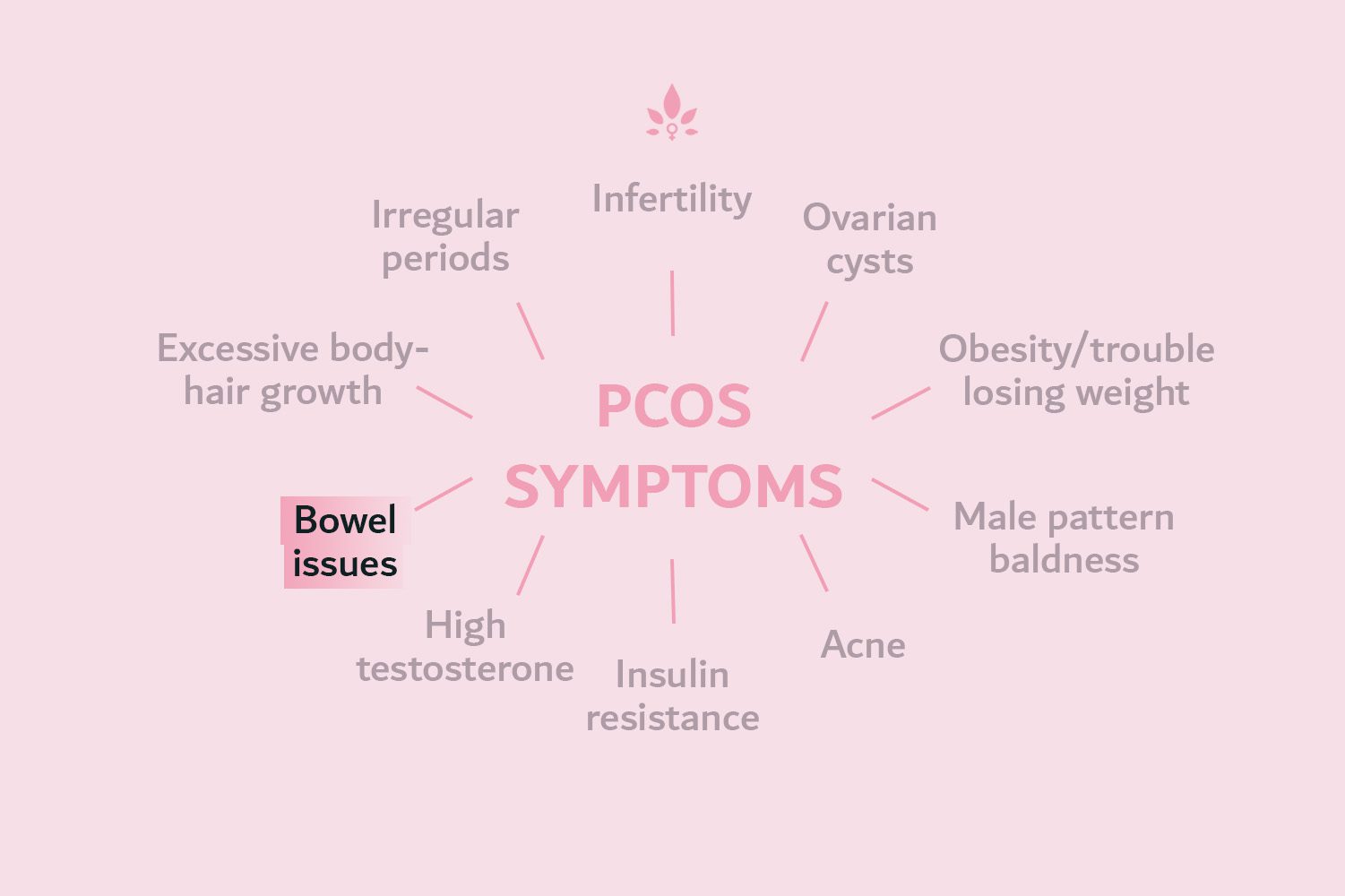
Polycystic ovary syndrome (PCOS) is a common hormonal disorder that affects women of reproductive age. It is caused by a hormonal imbalance in the body and can lead to a number of symptoms, including irregular menstrual periods, excess hair growth, acne, and weight gain. While urinary and bowel issues are not typically considered common symptoms of PCOS, they can occur in some individuals with the condition.
The most common urinary symptom associated with PCOS is urinary tract infections (UTIs), which can cause symptoms such as frequent or urgent urination, pain or burning during urination, and cloudy or bloody urine. These symptoms can be treated with antibiotics.
- PCOS cause urinary and bowel issues even when women have non-classic PCOS.
- This is because the cysts may press against the bladder and rectum (bowel).
- Cysts can be removed under general anaesthetic.
- PCOS symptoms can be relieved through changing your lifestyle.
Classic and Non-Classic PCOS
Despite its name, polycystic ovary syndrome does not require the presence of polycystic ovaries. In fact, when present together, excess of male hormones (hyperandrogenism) and lack of ovulation (anovulation) comprise the classic form of PCOS, which is more common and generally associated with more severe side effects than the non-classic form.
Women who have non-classic PCOS can have polycystic ovaries with regular menstrual cycles and hyperandrogenism (non-classic ovulatory PCOS). Or they can have normal androgens but experience chronic anovulation (non-classic mild/normoandrogenic PCOS).
PCOS Can Cause Urinary and Bowel Issues
Although non-classic PCOS is typically milder, those women who have extensive ovarian cysts may experience pain in the pelvic region where the cysts press against the bladder and rectum. Associated symptoms include nausea, urinary conditions, and constipation.
Depending on the severity of the symptoms, treatment options range from over-the-counter pain relief medication to cyst removal under general anaesthetic. Ultrasound investigation will be used to establish how invasive the cysts are.
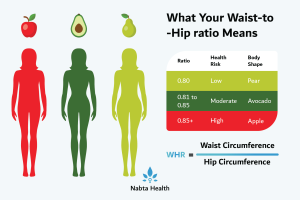
In addition to the pain and pressure caused by the presence of cysts in the abdominal region, many women with PCOS experience symptoms that are usually associated with diabetes. This is probably because a large proportion of women with the condition are insulin resistant.
Symptoms such as sugar cravings, frequent urination, blurred vision, delayed healing, and a tingling sensation have all been reported.
To date, the most effective way of relieving the symptoms of PCOS is through the implementation of lifestyle changes, such as weight loss.
What are the common urinary and bowel symptoms associated with PCOS?
- Polycystic ovary syndrome (PCOS) is a common hormonal disorder that affects women of reproductive age.
- It is caused by a hormonal imbalance in the body and can lead to a number of symptoms, including irregular menstrual periods, excess hair growth, acne, and weight gain.
- While urinary and bowel issues are not typically considered common symptoms of PCOS, they can occur in some individuals with the condition.
- The most common urinary symptom associated with PCOS is urinary tract infections (UTIs), which can cause symptoms such as frequent or urgent urination, pain or burning during urination, and cloudy or bloody urine.
- Another urinary issue that can occur with PCOS is incontinence, or the inability to control the release of urine from the bladder.
- Constipation is a common symptom of PCOS. This can be caused by hormonal imbalances and changes in the levels of insulin and other hormones in the body.
- It’s important to talk to a doctor if you have PCOS and are experiencing any symptoms related to your urinary or bowel health. They can help diagnose and treat any underlying issues and provide you with the care and support you need to manage your condition.
To read more about factors that are associated with PCOS click here and consider Nabta’s PCOS Test to understand more.
Nabta is reshaping women’s healthcare. We support women with their personal health journeys, from everyday wellbeing to the uniquely female experiences of fertility, pregnancy, and menopause.
Get in touch if you have any questions about this article or any aspect of women’s health. We’re here for you.
FAQ’s On PCOS Cause Urinary and Bowel Issues?
Can PCOS Cause Blood In Urine
Yes, Polycystic Ovary Syndrome (PCOS) can indirectly cause blood in urine due to associated conditions like urinary tract infections (UTIs) or kidney issues. It’s important to consult a healthcare provider for an accurate diagnosis and appropriate treatment.
PCOS Urine Color
PCOS does not usually change urine color directly. However, related conditions such as UTIs or dehydration can cause urine to appear darker, cloudy, or bloody. Consult a healthcare provider if you notice unusual changes in urine color.
Does PCOS Cause You To Pee a Lot
Yes, PCOS can cause you to pee a lot due to related conditions like insulin resistance or diabetes, which can increase thirst and urination. It’s essential to consult a healthcare provider for proper diagnosis and management.
Can PCOS Cause UTI
Yes, PCOS can increase the risk of urinary tract infections (UTIs) due to hormonal imbalances and insulin resistance. It’s important to consult a healthcare provider for proper diagnosis and treatment.
PCOS Peeing a Lot
Yes, PCOS can cause frequent urination due to associated conditions like insulin resistance or diabetes, which can lead to increased thirst and urination. Consult a healthcare provider for proper diagnosis and management.
Sources:
El Hayak, S, et al. “Poly Cystic Ovarian Syndrome: An Updated Overview.” Frontiers in Physiology, vol. 7, 5 Apr. 2016, p. 124., doi:10.3389/fphys.2016.00124.
Norman, R J, et al. “The Role of Lifestyle Modification in Polycystic Ovary Syndrome.” Trends in Endocrinology and Metabolism, vol. 13, no. 6, Aug. 2002, pp. 251–257.
Patel, S. “Polycystic Ovary Syndrome (PCOS), an Inflammatory, Systemic, Lifestyle Endocrinopathy.” The Journal of Steroid Biochemistry and Molecular Biology, vol. 182, Sept. 2018, pp. 27–36., doi:10.1016/j.jsbmb.2018.04.008.