ما هي العلاقة بين مُقاومة الأنسولين ومُتلازمة المبيض المُتعدد الكيسات؟

An increased sensitivity to insulin is very common in women who have classic PCOS. Classic PCOS is characterised by chronic anovulation and hyperandrogenism with or without polycystic ovaries. Women with classic PCOS are more likely to experience concurrent metabolic symptoms, the most common of which is insulin resistance.
Up to 85% of patients with PCOS have hyperinsulinemia. These patients are often borderline diabetic and are frequently overweight.
Increased insulin potentiates ovarian androgen production, which is a driving factor of hyperandrogenism. Insulin modulates ovarian steroidogenesis, which is the process by which the steroid hormones oestradiol and progesterone are synthesised from cholesterol. It is also involved in the control of ovulation, via an insulin signalling pathway in the central nervous system.
Treating insulin resistance
Insulin resistance is often treated with insulin sensitising drugs, such as metformin. Whilst this type of medication does not completely normalise circulating androgen levels, it can significantly reduce testosterone levels and has been used to successfully restore ovulatory menstrual cycles in some women with classic PCOS.
Another frequently prescribed medication for the treatment of PCOS is the oral contraceptive pill. This treatment is not suitable for those who are insulin resistant, as many forms of the pill impair insulin sensitivity. This means that, worryingly, the most widely used treatment for PCOS is probably unsuitable for the majority of women who exhibit the symptoms of the classic form of the condition. This should be discussed with your doctor prior to commencing treatment.
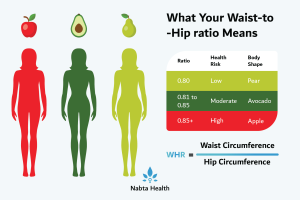
Fortunately, there is an alternative, which avoids prolonged use of medication (that may be doing more harm than good anyway). Lifestyle modifications in the form of diet adjustments, weight loss and reduced sugar intake, can help to rectify the symptoms of PCOS that are associated with insulin resistance. Studies have shown that as little as 5% weight loss can regulate the menstrual cycle and improve fertility. In fact, holistic lifestyle changes are now considered to be the most sustainable treatment approach for many patients with PCOS.
Alongside this, some women use dietary supplements in an attempt to relieve the symptoms of classic PCOS. Whilst a small number of studies have shown that magnesium supplements improve insulin resistance, further work is required to confirm if this is also the case in individuals with PCOS who are insulin resistant. Additional small-scale studies have demonstrated that co-supplementation of omega-3 fatty acids with vitamin E improved insulin resistance and reduced the levels of circulating testosterone in women with PCOS. Further work is required to substantiate the claim that omega-3 fatty acids may be a viable treatment option for PCOS.
Women who have PCOS and are insulin resistant need to find a way of managing their condition, not just for short term symptomatic relief, but also because they are predisposed to developing other conditions including metabolic syndrome, non-alcoholic fatty liver disease, gestational diabetes and pregnancy-induced hypertension.
Finally, women with non-classic PCOS who have normal ovulation and/or normal androgen levels, will usually only experience mild metabolic symptoms. They are less likely to be overweight and will often have normal insulin sensitivity. However, there is the possibility that extrinsic risk factors, such as weight gain, may cause their condition to convert to classic PCOS over time. Thus, a good diet and maintenance of a healthy weight is recommended for all women with PCOS.
To read more about factors that are associated with PCOS click here.
Nabta is reshaping women’s healthcare. We support women with their personal health journeys, from everyday wellbeing to the uniquely female experiences of fertility, pregnancy, and menopause.
Get in touch if you have any questions about this article or any aspect of women’s health. We’re here for you.
Sources:
- Diamanti-Kandarakis , E, and A Dunaif. “Insulin Resistance and the Polycystic Ovary Syndrome Revisited: An Update on Mechanisms and Implications.” Endocrine Reviews, vol. 33, no. 6, 1 Dec. 2012, pp. 981–1030., doi:10.1210/er.2011-1034.
- Ebrahimi, F A, et al. “The Effects of Omega-3 Fatty Acids and Vitamin E Co-Supplementation on Indices of Insulin Resistance and Hormonal Parameters in Patients with Polycystic Ovary Syndrome: A Randomized, Double-Blind, Placebo-Controlled Trial.” Experimental and Clinical Endocrinology & Diabetes , vol. 125, no. 6, June 2017, pp. 353–359., doi:10.1055/s-0042-117773.
- El Hayak, S, et al. “Poly Cystic Ovarian Syndrome: An Updated Overview.” Frontiers in Physiology, vol. 7, 5 Apr. 2016, p. 124., doi:10.3389/fphys.2016.00124.
- Marshall, J C, and A Dunaif. “Should All Women with PCOS Be Treated for Insulin Resistance?” Fertility and Sterility, vol. 97, no. 1, Jan. 2012, pp. 18–22., doi:10.1016/j.fertnstert.2011.11.036.
- Norman, R J, et al. “The Role of Lifestyle Modification in Polycystic Ovary Syndrome.” Trends in Endocrinology and Metabolism, vol. 13, no. 6, Aug. 2002, pp. 251–257.
- Patel, S. “Polycystic Ovary Syndrome (PCOS), an Inflammatory, Systemic, Lifestyle Endocrinopathy.” The Journal of Steroid Biochemistry and Molecular Biology, vol. 182, Sept. 2018, pp. 27–36., doi:10.1016/j.jsbmb.2018.04.008.
- Shokrpou, M, and Z Asemi. “The Effects of Magnesium and Vitamin E Co-Supplementation on Hormonal Status and Biomarkers of Inflammation and Oxidative Stress in Women with Polycystic Ovary Syndrome.” Biological Trace Element Research, 18 Dec. 2018, doi:doi: 10.1007/s12011-018-1602-9.